Dr. Birx, March 26, 2020.
redo Jump to...
print Print...
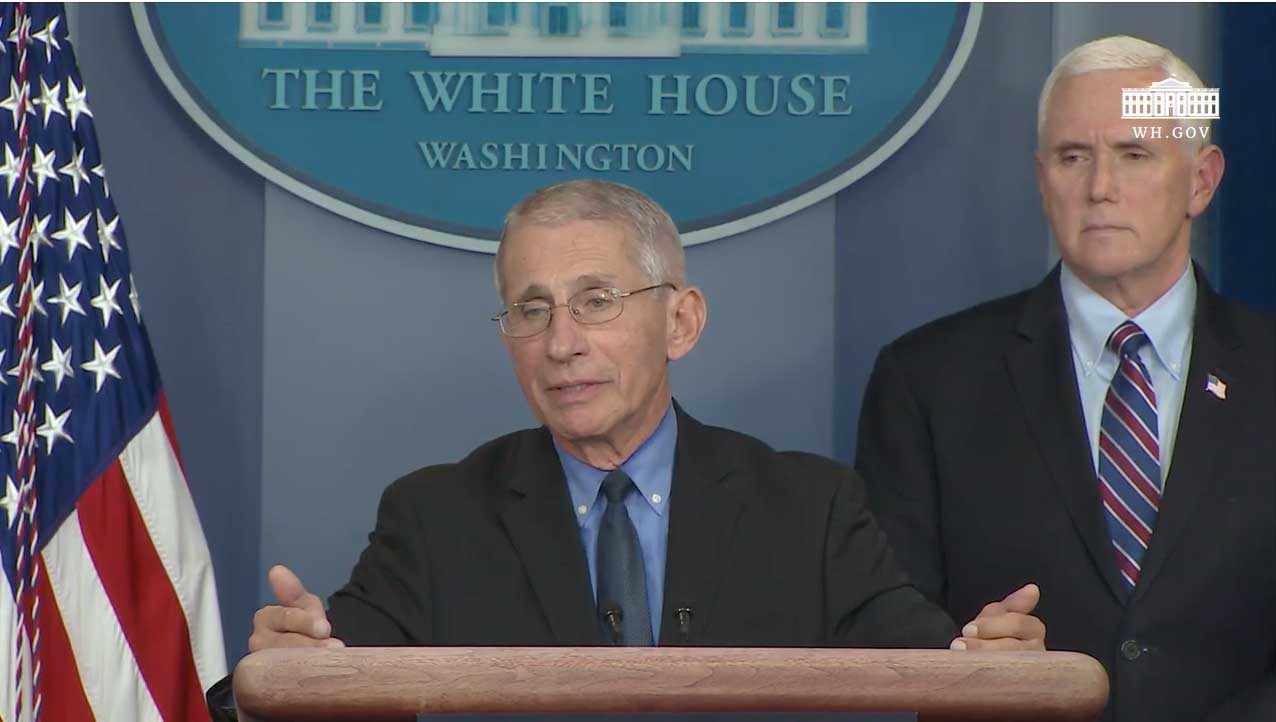
MARCH 26, 2020 WHITE HOUSE TASK FORCE PRESS BRIEFING: The following are remarks by Dr. Deborah Birx and Dr. Anthony Fauci:
VICE PRESIDENT PENCE: And now for information on the latest on data and what we’re seeing, Dr. Deborah Birx.
DR. BIRX: Thank you. Thank you, Mr. Vice President. So just as a summary of where it looks domestically — I won’t talk so much about the global issues this time: We do have 19 out of our 50 states, to be reminded, that had early cases but have persistently low level of cases and, at this point, have less than 200 cases. So that’s almost 40 percent of the country with extraordinarily low numbers.
And they are testing. Some of our governors have been very adamant about their need for test kits. We have gotten them test kits.
When we had Abbott add — about a week ago — to the test kits, we’ve been able to open up additional test kits for our states that want to do surveillance and want to do contact tracing. These 19 states are doing still active containment. There’re at 200 cases despite the fact that they’ve been measuring them over the last three to four weeks.
Still though, 55 percent all cases and 55 percent of all new cases continue out of the New York metro area; that’s the New Jersey part and New York part, in particular. I haven’t added in Connecticut or other counties at this point.
We are concerned about certain counties that look like they’re having a more rapid increase, if we look at Wayne County in Michigan and you look at Cook County in Chicago. So we have integrated all of our information to not only look at where the cases are today, but how they’re moving, so we can alert FEMA to where we think the next potential hotspot is. [*On March 19, President Trump announced FEMA would take over the government’s coronavirus response on the ground.]
All of the counties that I’ve mentioned — the hotspots are in urban areas or in the communities that serve that urban area. And I think that’s something very important to remember as we move forward.
Because of the innovations within our private sector, we continue to have these new platforms added for laboratory testing. And these become critical platforms for states that have very low rates and very low rates needed to test. Why is that important? Some of these machines have wells and plastic plates that, in order to be effective, you have to put on about almost 96 samples. And others are made for 4 samples or 24 samples at a time.
So what’s critical for us to be able to do is to match the need to the county and state. And that’s the role that we can provide advice on because we get to see across the whole country, and where those items are needed most. And so this is allowing us to adapt and adopt, really, allocation of tests or recommendations to state what piece of equipment they may need.
The 550,000 tests: You can do the math, but we’re still running somewhere about 14 percent overall. That means 86 percent of the people with significant symptoms — because remember, you had to have a fever and symptoms to get tested at this point — so, still 86 percent are negative. These are really important facts for the American people.
I’m sure many of you saw the recent report out of the UK about them adjusting completely their needs. This is really quite important. If you remember, that was the report that said there would be 500,000 deaths in the UK and 2.2 million deaths in the United States. They’ve adjusted that number in the UK to 20,000. So, half a million to 20,000. We’re looking into this in great detail to understand that adjustment.
I’m going to say something that’s a little bit complicated, but I’m going to try to do it in a way that we can all understand it together. In the model, either you have to have a large group of people who are asymptomatic, who have never presented for any test, in order to have the kind of numbers that were predicted to get to 60 million people infected or 6 million people infected. You have to have a large group of asymptomatics, because in no country to date have we seen an attack rate over 1 in 1,000.
So either we’re only measuring the tip of the iceberg of the symptomatic cases and underneath it are a large group of people. So we’re working very hard to get that antibody test because that’s a good way to figure out who are all these people under here and do they exist. Or we have the transmission completely wrong.
So these are the things we’re looking at because the predictions of the models don’t match the reality on the ground in either China, South Korea, or Italy.
We are about five times the size of Italy. So if we were Italy and you did all those divisions, Italy should have close to 400,000 deaths. They’re not close to achieving that. So these are the kinds of things we’re trying to understand. Models are models. We’re adapting now to the — there’s enough data now of the real experience with the coronavirus on the ground to really make these predictions much more sound.
So when people start talking about 20 percent of a population getting infected, it’s very scary. But we don’t have data that matches that, based on the experience.
And then, finally, the situation about ventilators. We were reassured, in meeting with our colleagues in New York, that there are still ICU beds remaining and there’s still significant — over 1,000 or 2,000 — ventilators that have not been utilized yet.
[Dr. Birx is speaking directly to the reporters here]: Please, for the reassurance of people around the world — to wake up this morning and look at people talking about creating DNR situations — do-not-resuscitate situations — for patients, there is no situation in the United States right now that warrants that kind of discussion. You can be thinking about it in a hospital — certainly many hospitals talk about this on a daily basis — but to say that to the American people, to make the implication that when they need a hospital bed, it’s not going to be there, or when they need that ventilator, it’s not going to be there — we don’t have evidence of that right now. And it’s our job collectively to assure the American people that — it’s our collective job to make sure that doesn’t happen.
Right now, you can see these state — these cases are concentrated in highly urban areas. There are other parts of the states that have lots of ventilators and other parts of New York State that don’t have any infections right now.
So we can be creative. We can meet the need by being responsive. But there’s no model right now — I mean, no reality on the ground where we can see that 60 to 70 percent of Americans are going to get infected in the next 8 to 12 weeks. I just want to be clear about that.
So we’re adapting to the reality on the ground. We’re looking at the models of how they can inform. But we also are learning very clearly from South Korea and from Italy and from Spain.
Just to — because I know many of you will look up my numbers — the only people who are over, really, 1 in 1,000 cases are people that have very small populations, like Monaco and Liechtenstein. So you will see a different number coming from when your population is really tiny; one case can put you over 1 to 1,000 or 2 to 1,000. Thank you.
THE VICE PRESIDENT: Good. We’ll do questions in a moment. Dr. Fauci.
DR. FAUCI: Thank you Mr. Vice President. I’m going to change the topic just a little bit because there was questions that came up and I’ve been asked about this on a couple of media interactions regarding the interventions that we’re talking about. And it’s important because it’s about something that I said yesterday, about what we would likely see.
Whenever you put the clamps down and shut things down, you do it for two reasons: You do it to prevent the further spread — as we call, mitigation — but you also do it to buy yourself time to get better prepared for what might be a rebound. It may be a rebound that we get things really under control, and then you pull back, which ultimately we’re going to have to do. Everybody in the world is going to have to do that. You’re either going to get a rebound, or it might cycle into the next season.
So what are we going to do to prepare ourselves for that? One of the most important things is one that I mentioned several times from this podium, and that is to clarify a bit about the timeline for vaccines and would that have any real impact on what we would call “the rebound” or what we call a “cycling in the season.”
Certainly, for sure, a vaccine is not going to help us now, next month, the month after. But as I mentioned to you, we went into a phase one trial. And I keep referring to one vaccine; there’s more than one. There’s a couple of handfuls of vaccines at different stages of development, but they’re all following the same course. And the course is: You first go into a phase one trial to see if it’s safe and you have very few people, 45 people, within a certain age group — all healthy, none at really any great risk of getting infected. And the reason you do that is because you want to make sure that it’s safe.
Then the next thing you do — and that takes about three months, easily, maybe more. So that’s going to bring us into the beginning or middle of the summer.
Then you go to a phase two trial, or what we say “two-three,” which means we’re going to put a lot of people in there. Now we hope that there aren’t a lot of people getting infected, but it is likely there will be somewhere in the world where that’s going on. So it’s likely that we will get what’s called an “efficacy signal,” and we will know whether or not it actually works.
If, in fact, it does, we hope to rush it to be able to have some impact on recycling in the next season. And like I said, that could be a year to a year and a half. I’m not changing any of the dates that I mentioned.
But one of the things that we are going to do that you need to understand — that has been a stumbling block for previous development of vaccines — and that is, even before you know something works, at risk, you have to start producing it. Because once you know it works, you can’t say, “Great, it works. Now give me another six months to produce it.” So we’re working with a variety of companies to take that risk. We didn’t take it with Zika. That’s why, you know, we have a nice Zika vaccine but we don’t have enough to do it because there’s no Zika around. Same with SARS. So that’s one of the things we’re really going to push on is to be able to have it ready, if in fact, it works.
Now, the issue of safety — something that I want to make sure the American public understand: It’s not only safety when you inject somebody and they get maybe an idiosyncratic reaction, they get a little allergic reaction, they get pain. There’s safety associated — “Does the vaccine make you worse?” And there are diseases in which you vaccinate someone, they get infected with what you’re trying to protect them with, and you actually enhance the infection. You can get a good feel for that in animal models. So that’s going to be interspersed at the same time that we’re testing. We’re going to try and make sure we don’t have enhancement.
So the worst possible thing you do is vaccinate somebody to prevent infection and actually make them worse.
Next, and finally, with regard — I’ll get you — to your question. Finally, with regard to therapies — I mean, we keep getting asked about therapies. There’s a whole menu of therapies that are going into clinical trial. As I’ve told you all and I’ll repeat it again: The best way to get the best drug as quickly as possible is to do a randomized controlled trial so that you know is it safe and is it effective. If it’s not effective, get it off the board and go to the next thing. If it is effective, get it out to the people that need it.
So you’re going to be hearing, over the next month or more, about different drugs that are going to go into these randomized controlled trials. And I feel confident, knowing about what this virus is and what we can do with it, that we will have some sort of therapy that’ll give at least a partial, if not a very good protection in preventing progression of disease. And we’ll be back here talking about that a lot, I’m sure.
Thank you. (**See “Background” below for the Q&A with reporters following Dr. Birx and Dr. Fauci’s remarks.)
Watch the video:
Questions
NOTE TO STUDENTS:
- President Trump and members of the White House Coronavirus Task Force have been giving daily press briefings followed by Q&A with reporters.
- During Thursday’s press briefing, Dr. Deborah Birx, Response coordinator for the Task Force, who is also the Global AIDS Coordinator, and Dr. Anthony Fauci, Director of the National Institute of Allergy and Infectious Diseases, made several points important for all Americans to understand regarding the spread of the virus, the number of cases, the number of ventilators needed, vaccines and treatment (therapies).
**WATCH THE VIDEO OF THEIR REMARKS ABOVE
1. a) How many states have less than 200 confirmed cases of coronavirus?
b) What did Dr. Birx emphasize about these numbers?
2. Where are the majority of coronavirus cases in the U.S.?
3. What did Dr. Birx note about the counties having a more rapid increase in cases?
4. What is important to note about the number of people being tested who come back positive for the coronavirus, according to Dr. Birx?
5. a) How did the UK experts who projected a certain number of cases and deaths change their prediction?
b) Ask a parent: what do you take away from this information?
6. a) What important points did Dr. Birx make about experts’ predictions of the models in China, South Korea, or Italy?
b) What does she say about the prediction that 20% of the population will get coronavirus?
7. What do you think about Dr. Birx’s assurance about ventilators? (see para. 16-17)
8. What different approach to vaccines does Dr. Fauci say they will be taking in addressing the coronavirus?
Background
Read the full text of the March 26 Task Force press briefing at whitehouse.gov. and watch the entire video at: the White House youtube page.
Following Dr. Birx and Dr. Fauci’s remarks, they took questions from the reporters. (They are also included in the video above.)
THE VICE PRESIDENT: Tony, if you want, you can take a question. Go ahead.
Q If I could just get back to what you’re saying about this idea of risk in drug manufacture. Are you saying that at some point in the phase two trials, that if you’re seeing some form of efficacy, that you may try to convince a laboratory to spool up production at that point so that there is a reservoir on hand?
FAUCI: Even before.
Q Even before.
FAUCI: When I go into phase two, I want to find somebody that is going to make it.
Q And who would pay for that?
FAUCI: Well, partially the federal government, I think, in some respects, to de-risk it, but also investments by the companies. A lot of companies are not shy now about doing that. Usually, when you do that at risk, John, you’ve got to give some backup for them, and we’ve done that. We’ve put hundreds of millions of dollars into companies to try and make vaccines. I wouldn’t hesitate to do that for a moment now.
Q On the county issue, I was talking about having low-risk, medium-risk, and high-risk counties — or for Dr. Birx — but there is no domestic travel restrictions. What’s to prevent somebody from a high-risk county going to a low-risk county? Don’t you risk creating a patchwork system, allowing more cases to slip through the cracks and the virus to spread in other areas of the country?
BIRX: I think this is a very important concept and it’s why we’ve really worked on messaging to the American people about these “15 Days to Stop the Spread,” because part of this will be the need to have highly responsible behavior between counties. And I think the American people can understand that — that they will understand where the virus is because we’ll have the testing data and where it isn’t, and make sure that they’re taking appropriate precautions as they move in and out of spaces.I think this will be critical for our future as we work together to really understand where the virus is and where it isn’t in real time.
Q Dr. Birx, if I could just follow up on, sort of, your modeling. Everyone is talking about this Neil Ferguson study out of Imperial and how the modeling has changed. You, last week, said — or it was on Monday that you talked about a serology test, something promising coming out of Singapore. Where are we on a serology test? The President said “very quickly.” And then is that what you need to do some sort of community survey, so you can get to some of these Xs and Zs so you can figure this all out?
BIRX: So we’re talking to CDC right now. They are extraordinary in outbreaks and contact tracing. So they are going to be the workforce behind any new strategy that looks at counties that need to completely move into containment and surveillance and contact tracing. But part of what they’re looking at now is where are these antibody assays. To be clear, there is antibody assays available right now, but they’re by ELISA. And what we’re trying to do is not just do ELISAs because they can use that now, but to be able to have point-of-care rapid diagnostics like we have with HIV — where you just get a drop of blood, you put it on a little cassette, and it tells you if you’re positive or negative. So that’s what companies are working on.
Q That’s the IgG? The —
BIRX: Yes, correct. That’s the IgG to measure. Now, remember, that’s not going to be helpful in diagnosis.
Q But that will get you —
BIRX: That’s going to be helpful for us to know how many asymptomatic cases there are — or were.
Q How close are we to figuring out what the asymptomatic rates are? Because that seems to be the big question here on where we are on the iceberg.
BIRX: It is a big question. It is a very big question. And so we have people — the FDA is working on that around the clock. They do have applications that are coming in. We put out a call for applications. I’ve been talking about it from this podium. If you have an IgG assay rapid test, not an ELISA — I mean, you could do the ELISA today because the SARS — the original SARS antigens react very well to the current COVID-19 antibodies that people have. But we’re really working on that, both so that we could have therapeutics that could be plasma-derived. So, thank you. Yes we’re very much focused on that.
Q Dr. Birx, how soon will you be able to — how soon will you be able to classify these counties? Because there’s a lot of testing that has not been done there.
BIRX: Well, you know, there are states — and I just want to really recognize state and local health officials that, behind all of this, have continued to test and have continued to do surveillance. So we do have states that have been doing surveillance all along, who have been doing contact tracing all along. It never gets reported because it’s not — you know, it’s not that exciting that they’ve identified 10 cases. But there are states doing that and have been doing it throughout this entire outbreak, and that’s why we have some confidence that that testing has been going on.
We have to expand testing for surveillance. But this is that — we talked about a little bit yesterday: the flu platform. So the flu platform is driven off of emergency rooms and hospitals reporting flu-like illness to their state and local governments, and that then will trigger the individuals to get tested.
So we have a platform that states and local governments are completely used to. They’re not used to doing it this late in the season. They’ll do it usually through the end of March, but flu usually tails off a lot by April. So we’re asking them to continue the activation of screening for flu-like illness.
Now, that doesn’t get to his question about where’s the asymptomatics and how much of that. That helps us find cases and contact trace on systematic cases.
Q So will there be different guidance for the places, the counties that don’t have the data yet? Will there be different CDC guidelines?
BIRX: So these are very early days of us trying to –what we’re trying to do is to utilize a laser-focused approach rather than a generic horizontal approach. And I think, in the 21st century, we should be able to get to that.
Why am I confident that we can do that? Because we do that in Sub-Saharan Africa right now for HIV. That’s how we’re stopping the epidemic there.
So we’ve done it. We’ve done it in resource-limited settings. So I do believe we can transpose that approach here to the United States and be able to have — we have granular data down to a GPS coordinate of a site of a clinic and hospital. We think that same thing can be done in the United States.
Q Dr. Birx, quick question on the restrict- — when you suggest restrictions to states for something like that — like, if there’s a high-risk county, and the restaurants are open in a low-risk county, wouldn’t your fear be that people in that high-risk county go over to the restaurants that are open there?
BIRX: So these are dialogues that the federal government has to have with state and local governments because state and local governments make those decisions. And that’s what’s been inspirational to me, is seeing how much the governors understand where they are in their epidemic and what they will need to do in the future.
This is what we’re trying to tailor. It requires us to have very clear data disaggregation at the county and state level. But I think you’ve been hearing from us — these outbreaks and clusters, we’ve been able to very well define to date: the one that was in King County, the one that is now in New York City, the one in New Orleans, the one in Wayne County. So — and we can see that spread throughout the region and as closely related counties.
So this is what we’re talking about: how to do surveillance, how to do contact tracing, and how to do each of these items to make sure that you prevent that spread.
Q What’s your timeline, do you think? What’s your timeline for implementing guidance like this?
BIRX: Well, we have to get all of our data together. We owe it to the President. And we owe it to the President to be able to make that decision, so that’s what we’re working on right now, is getting that granularity.
Daily “Answers” emails are provided for Daily News Articles, Tuesday’s World Events and Friday’s News Quiz.